INTRODUCTION
The occurrence of cesarean deliveries in countries such as Egypt in the year 2014 (50.6%), was observed to have surpassed the World Health Organization (WHO) recommend.1
Many operations are now-a-days done simultaneously with cesarean sections, with different success rates and complications. These operations may be gynecological or nongynecological as shown in Figure 1.
Figure 1: Types of Surgeries that could be done in Association with Cesarean Delivery.

GYNECOLOGICAL SURGERIES
Uterine Surgeries with Cesarean Section
Myomectomy
Myomectomy during cesarean section is limited only to pedunculated myomas, because resection of myomas at the time of cesarean section usually stimulates profuse bleeding, requiring life-saving hysterectomy.2-4
Many researchers have studied the feasibility of myomectomy during cesarean section, either by developing new techniques for myomectomy or by devascularization techniques to reduce blood loss and to potentially eliminate multiple surgeries. However, many surgeons are still resisting this policy due to the lack conclusive evidence demonstrating its safety.5
Incebiyik et al6 conducted a retrospective study including 16 patients who underwent myomectomy, concurrently with cesarean section, between January 2009 and September 2012. The pre- and post-operative hemoglobin values, number, size and total volume of excised fibroid nodules, location of fibroids, duration of operation, and duration of hospital stay of all patients were retrospectively investigated. They concluded that, myomectomy carried out during cesarean section is a safe surgical intervention regardless of the size of leiomyomata.
Awoleke et al7 conducted a review study on myomectomy during cesarean section in Africa, with respect to the duration of surgery, blood loss, length of hospital stay, and blood transfusions. He found a limited number of studies in this issue owing to the fear of complications; however, the authors of the published studies concluded that the complications and morbidity following cesarean myomectomy do not significantly differ from those occurring during cesarean section alone, while fertility is apparently not compromised by this treatment. Success of procedure requires careful patient selection, adequate experience, and efficient haemostatic measures.
Simsek et al8 conducted a retrospective study on 70 patients of cesarean myomectomy (Group 1) and compared the results with patients who underwent cesarean section alone (Group 2). The mean surgical time of the myomectomy Group was 58.1+/-23 minutes which was significantly increased (p<0.01). Mean post-operative hemoglobin value was 9.6+/-1.5 in the myomectomy Group and 10.8+/-1.01 in controls (p=0.01). Length of hospital stay was significantly longer in the myomectomy Group (p<0.05). Although, the procedure was related with increased blood loss, authors concluded that myomectomy during cesarean section is a feasible procedure without any serious
complications or the need for blood transfusion.
Lee et al9 conducted a study on 31 patients where myomectomy was performed during cesarean section. They developed a new purse-string suture allocated around myoma during cesarean section with the assistant maintaining strong tension on the purse-string suture around the myoma. They concluded that, purse-string suture method was effective and safe for more than 3 years and have not observed failures and serious complications, such as late hemorrhage and uterine rupture during a subsequent pregnancy.
Sapmaz et al10 conducted a prospective study on 70 patients who underwent cesarean myomectomy, allocated in 2 Groups. The Group I included 52 patients who underwent cesarean myomectomy with systemic devascularization while Group II included 18 patients managed by tourniquet and served as a control. They stated that bilateral ascending uterine artery ligation and tourniquet use had similar outcomes with regard to intraoperative blood loss in cesarean myomectomy cases; however, the efficacy of ligation on blood loss in the postoperative period is superior to tourniquet method, since the tourniquet is removed at the end of the operation. Therefore, bilateral ascending uterine artery ligation may be preferable in cesarean myomectomy cases.
Desaiet al11 used a novel technique of uterine devascularization in 17 patients before performing cesarean myomectomy, where the ascending and descending uterine arteries were ligated. Also, ligation of ovarian vessels, medial to the ovary was done. Not all patients required hysterectomy. No serious complications occurred and patients were discharged by the fifth day.
Holub et al12 assessed pregnancy outcomes and deliveries after laparoscopic ligation of uterine artery during laparoscopic myomectomy. One hundred and fifty-three patients underwent ligation and transection of uterine arteries in that four-year study. The study concluded that laparoscopic transection of uterine vessels preserves the uterus, maintains ovarian blood supply and allows for the achievement of pregnancy in women with symptomatic fibroids. Fetal growth and umbilical Doppler findings remained normal in all cases.
The conclusion was that, with a good patient selection and expertise, cesarean myomectomy is safe and feasible.13-22
Intra-Uterine Devices (IUD) Insertion During Cesarean Section
Many researchers found that intra-cesarean section Intra-uterine devices (IUD) placement is better than interval insertion after 6 weeks, with comparable expulsion rates. Blumenthal and Gold thwaite23 highlighted the numerous benefits of intra-operative IUD placement, including proper access to the uterine and no additional cost or duration to the primary delivery procedure.23
Pelayo et al24 conducted a prospective study which included 152 patients who underwent cesarean section. IUD were inserted in seventy-two patients during cesarean section, whereas the remaining 74 patients underwent cesarean section without IUD. Analysis of pain, bleeding and infection was done. Authors concluded that no difference in the results between both Groups was noticed and they recommended the insertion of the IUD during the cesarean section as a secure and helpful method for the fertility.
This was supported by the results of Halder et al25 who evaluated and compared the safety and efficacy of vaginal and intra-cesarean insertion of post-partum intrauterine contraceptive device. They found that both modes of insertion were found to have very low rates of expulsion, vaginal bleeding, infection, missing strings, and also effective as contraceptive. Expulsion rate was 4% in the vaginal Group and 2 % in intra-cesarean Group. They concluded that, intra-cesarean IUD insertion is an appealing approach for post-partum contraception after cesarean delivery.
On the other hand, a study done by Sevki et al26 concluded that insertion of IUD during cesarean section provides adequate protection against pregnancy. However, more than one fourth of the participants discontinued IUD use due to spontaneous expulsion or other medical reasons. Further studies concluded that, expulsion rate is higher with IUD insertion during cesarean section.27 Other studies provided the solution of expulsion by either anchoring methods or by the use of frameless IUD.28-30
At the end of this section, it can be concluded that, the quality of evidence was moderate and trials of adequate power are needed to estimate expulsion rates and side effects. The benefit of effective contraception immediately after delivery may outweigh the disadvantage of increased risk for expulsion.31
Cesarean Hysterectomy
Cesarean hysterectomy is suggested mainly to prevent or treat postpartum hemorrhage due to uterine atony, placenta accreta, percreta invading bladder minimizing blood loss and saving the mother’s life.32 American College of Obstetricians and Gynecologists (ACOG) advised elective planned cesarean hysterectomy without any trial to remove the placenta, to minimize the risks associated with placenta accreta such as massive bleeding and associated risks of disseminated intravascular coagulation, infection, acute respiratory distress syndrome, renal failure, and death.33
Shellhaas et al34 conducted a prospective, 2-year observational study at 13 academic medical centers between January 1, 1999, and December 31, 2000, on all women who underwent a cesarean hysterectomy. They found that 39,244 women underwent cesarean delivery with a total of 186 cesarean hysterectomies (0.5%). The causes for cesarean hysterectomy were: Placenta accreta (38%) and uterine atony (34%). The major complications associated with cesarean hysterectomy were: Blood transfusion (84%) and other blood products (34%), fever (11%), subsequent laparotomy (4%), ureteral injury (3%), and death (1.6%). Urinary complications were higher in cases of placenta accreta.
Another reason for peripartum hysterectomy was uterine rupture, either after vaginal delivery trial or due to previously scared uterus. Hysterectomy was indicated if hemorrhage persisted. Hysterectomy was either total or sub-total, depending on the site of rupture and the patient’s condition.35
Cesarean Radical Hysterectomy
Another reason for cesarean hysterectomy is cancer during pregnancy which poses significant challenges to both the clinician and the mother. This is usually observed in pregnant women in forties, when the incidence of some of the common malignant neoplasm begins to arise. Although, pregnancy is characterized by extensive medical observation, a delay in diagnosis and lack of attention to the subtle presentation of malignancies, could lead to such cases.36
Some authors advocate intrapartum hysterectomy (following either vaginal or cesarean birth) to be performed for patients with carcinoma in situ (CIS) or adenocarcinoma in situ (AIS) who have completed their families and/or have proved to be noncompliant. Although, postpartum regression may occur with even CIS, some surgeons argue against the routine performance of an intrapartum hysterectomy for the management of cervical intraepithelial neoplasia (CIN) in pregnancy.36
Monk and Montz et al37 studied the treatment of invasive cervical cancer, complicating intra-uterine pregnancy with radical hysterectomy. They identified 13 patients who underwent radical hysterectomy and bilateral pelvic lymphadenectomy with the fetus in situ and 8 others who underwent cesarean delivery followed by radical hysterectomy and bilateral pelvic lymph node dissection. The mean operative time was 281 minutes, and the mean blood loss was 777 mL for radical hysterectomy with the fetus in situ plus lymphadenectomy and 1750 mL when cesarean section preceded the cancer operation. The surgical morbidity was minimal for the whole Group, and after documentation of fetal maturation, seven healthy infants were delivered.37
Extra-Uterine Surgeries with Cesarean Section
Tubal sterilization
The most common operation done with cesarean section is tubal sterilization. Some patients, who have delivered vaginally before, prefer to undergo cesarean sterilization during the lastpregnancy.38
Ozyer et al39 conducted a study on 50 patients divided into 2 Groups, where Group I included 24 patients who had undergone tubal sterilization with cesarean delivery and Group II included 26 patients who had undergone tubal sterilization as a separate operation. They concluded that, tubal sterilization during cesarean section is more practical and safe than planned tubal sterilization alone.
Basava et al40 conducted a study on five hundred multigravid women who underwent Cesarean section for various reasons and wanted concurrent tubal sterilization by either modified Pomeroy’s technique or by Falope ring application. They reported one case of ectopic pregnancy with serious complications in a patient who underwent tubal sterilization by modified Pomeroy’s technique.
Swendeet al41 conducted a retrospective analysis of the clinical records of 78 patients who had undergone female sterilization in Makurdi. They concluded that a majority of female sterilization procedures were performed using cesarean section. The procedure was found to be safe and effective.
Salpingectomy
A retrospective analytical study was conducted at a tertiary care center from January 2010 to December 2014, in the Karnataka Institute of Medical Sciences, Hubli, Karnataka. The case files of all the patients who underwent the sterilization were taken from the medical records section and reviewed in detail. The cases were Grouped as cesarean tubectomy, minilaparotomy and laparoscopic sterilization, based on the technique used for abdominal entry. Out of 5442 cases of female sterilization, 2872 underwent cesarean tubectomy, while the remaining underwent minilaparotomy (1306) and laparoscopic sterilization (1264). They concluded that cesarean tubectomy is a safe and popular method, with more than half of the patients opting for it. Cesarean tubectomy can be offered to patients who undergo cesarean operation for obstetric indications and who desire a permanent method of sterilization.42
Another retrospective cohort study was conducted on women who underwent cesarean section performed in a single institution from December 2014 to January 2016. Operative reports were reviewed to confirm complete salpingectomy. A total of 171 patients were identified, who delivered via cesarean section with 50% of these patients proceeding with salpingectomy at the time of delivery. The salpingectomy completion rate was 96.4%. They concluded that salpingectomy at the time of cesarean delivery is feasible. Results from this study can be considered when managing a patient who desires sterilization and may also benefit from ovarian cancer risk reduction.43 The same results were supported by Danis et al44 who advised bilateral tubectomy at the time of cesarean section in the special population.
The shortcoming was that, with most cesarean deliveries, the removed segment of the fallopian tube is not examined for a histological diagnosis. Accordingly, it is important for the surgeon to verify the pathology report, which adds an additional component to the post-service work. The risks concerning the operative complications with this procedure are low, but real. The common risks are the failure to reach both tubes from extensive adhesions and broad ligament hematoma. Furthermore, sterilization failure occurs in about 1 in 100 cases even though the operation was performed properly. This failure also carries a liability risk. For the previously mentioned risks, FIGO does not approve of tubal sterilization during Cesarean section.45,46
Despite the ban of tubal sterilization by law in some countries, sterilizations continue to be performed during cesarean sections. The cause of the ban being that, cesarean sterilization contributes to the increase in cesarean sections.47
Ovarian Cystectomy
The reported incidents of adnexal masses during pregnancy vary from 1 in 81 pregnancies to 1 in 8000 pregnancies. There is still a debate regarding the management of incidental adnexal masses during the cesarean section considering the risk of this additional procedure on post-operative morbidity and mortality.48
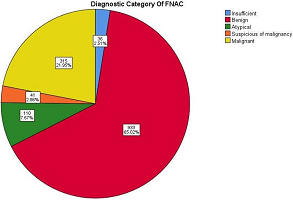
Hobeika et al48 reviewed the histopathology of 43 adnexal masses, incidentally diagnosed and excised during cesarean delivery. The histopathological diagnoses were: Mature cystic teratomas (34.9%), mucinous cystadenomas (16.3%) and serous cysts or cystadenomas (14.0%). Other histopathologies included: Endometriomas (11.6%), luteomas (7.0%), paraovarian cysts (4.7%), corpus luteum cyst (2.3%), fibroma (2.3%), inclusion cyst (2.3%), serous-mucinous cyst (2.3%) and borderline serous cystadenoma (2.3%). The authors concluded that ovarian tumors incidentally diagnosed and excised during cesarean delivery are rare and mostly benign. Also excision of such lesions should be considered.
Cengizet al49 conducted a retrospective study by reviewing medical records of the patients who had incidental adnexal masses during cesarean section in Istanbul, Turkey. There were 38 cases of incidental adnexal masses which were discovered during the cesarean section. The most common histological diagnosis was paraovarian-paratubal cysts with the rate of 23.7% (n=9). Cystectomy procedure during the cesarean section did not alter the morbidity of the patient.
Baseret al50 conducted a retrospective study during the period 2007-2012 on patients who were incidentally diagnosed with adnexal masses while undergoing cesarean section. The patients were surgically managed during cesarean delivery. Clinicopathological characteristics, maternal and neonatal outcomes were assessed. They concluded that, adnexal masses encountered during the cesarean delivery generally have a favorable prognosis in terms of maternal and fetal outcome.
Another retrospective study conducted in France, at Lille University Hospital between 1st January 2007 and 31st December 2010. They found that 12 operations for ovarian masses were performed during cesarean section. Operated cysts were most often organic cysts (74.39%). No malignancies were observed, and 3 cases of borderline tumors were diagnosed. There were no obstetrical or neonatal complications (Figure 2).51
Figure 2: Ovarian Cystectomy during Cesarean Section.

NON- GYNECOLOGICAL SURGERIES
Intraperitoneal Operations
Appendectomy
has a non-classical presentation in pregnancy and can occur in the late third trimester. To avoid the risk of future appendicitis occurrence, some surgeons have advocated and performed elective appendectomy at CS (Figure 3) as an acute presentation of this syndrome has a high risk of complications.52-54
Figure 3: Appendectomy and Tubal Sterilization during Cesarean Delivery.

Continuous spinal anesthesia was developed by facilitate bilateral tubal ligation and appendectomy. Studies have confirmed the safety of performing incidental appendectomy at the time of cesarean section. The authors, therefore, propose that clinicians visualize and palpate the appendix at all cesarean sections, and remove those with evidence of inflammation or disease.55,56
Pearce et al54 performed appendectomy on 93 patients after receiving their written consent to undergo elective cesarean section in a clinic population. The parameters assessed were clinical infection, blood loss, and gastrointestinal tract recovery rates. They found that these parameters were equal in both Groups. Operative time was extended by 15 minutes to the total operation time and the hospital stay was extended by about 12 hours. There were no wound infections or serious morbidity. Prophylactic appendectomy in selected cases, such as women with abnormally appearing appendix, a history of pelvic pain, endometriosis, or anticipated intra-abdominal adhesions do not seem to add to the risk of elective cesarean section.
Systematic reviews were found to support appendectomy or elective appendectomy at cesarean section with no added risks or complications.57-59
Extra-Peritoneal Operations
Abdominoplasty
Abdominoplasty is an aesthetic surgical procedure that restores female figure and abdominal contouring. Multiparity and nonpregnancy spacing usually lead to lower abdominal skin redundancy and excess fat accumulation. Moreover, cesarean delivery results in weakness in the lower abdominal wall muscles. Recently, cases of women requesting abdominoplasty at the time of cesarean delivery has soared, since it eliminates the need for another surgery and reduces expenditure. Moreover, gynecologists are learning and upgrading their skills to perform aesthetic surgery, especially abdominoplasty along with cesarean delivery due to the increasing requests from patients.60
Ali and Essam61 conducted a study on 50 pregnant women from 2008 to 2009 who underwent abdominoplasty and limited liposuction at the same time with cesarean section in Kuwait. These cases were compared to 80 cases of abdominoplasty alone. It was found that wound infections, wound dehiscences, and distal skin necrosis were reported more often in women who underwent the combined procedure, than in the ones that underwent abdominoplasty alone. Moreover, the researchers noted that marking the pregnant abdomen was more difficult than the non-pregnant abdomen. Most patients (52%) were not satisfied by the results of combined surgery, where 32% of the patients reported bulging of the abdomen, 24% reported a bulging umbilicus and 12% reported recurrent abdominal skin redundancy. Only 48% of the women were satisfied with the overall results of combined surgery (abdominoplasty with cesarean section). They concluded that, abdominoplasty combined with cesarean delivery carries a higher risk of complications and does not give the desired aesthetic outcome. The authors do not recommend this practice. Thabet et al62 at Cairo University, Egypt had similar results and conclusions.
Teri et al60 conducted a review study to evaluate the evidence supporting the results of studies to evaluate abdominoplasty combined with cesarean section. They concluded that the quantity and quality of researches are inadequate and the results of these studies did not recommend a combination of abdominoplasty with cesarean section, as more complications occur, the cosmetic results being unsatisfactory and recurrence being more common.
Hence, concluding from the non-systematic reviews, the application of abdominoplasty combined with cesarean section should be discouraged.
Hernioplasty
Evaluation of the clinical outcome of inguinal or umbilical hernioplasty performed at the time of cesarean section, and comparison of the outcome of this Group with a control population, who underwent a cesarean section alone, was done retrospectively by Gabriele et al.63 No significant difference was found in the hospital stay, comparing 28 patients with 100 matched controls, who only underwent cesarean section. No complications were recorded during the perinatal and follow-up periods.
Chen et al64 reported the repair of diaphragmatic hernia following the emergency cesarean section, in which they found a part of the transverse colon and a part of omentum trapped in the thorax, through a 3 cm by 3 cm, by laceration in the patient’s diaphragm. They removed the trapped intestine which was about 40 cm in length and repaired the diaphragmatic hernia at the same time.
Abdominal wall hernia repair concomitant to cesarean section seems feasible and beneficial to the patient, as the current literature suggests no increased risk in pre or post-operative complications. Moreover, a combined procedure saves the patient from an additional operative procedure.65
On the other hand, a high rate of post-operative wound complications were reported, although, comparable to that following a standard elective cesarean section has been observed by some researchers.66,67
Evidence supports the combined procedure of cesarean section and hernia repair, thereby concluding that it is feasible and safe.65
CONCLUSIONS
Many surgeries could be performed safely in association with cesarean delivery within less time and minimal blood loss. The perspective towards the concept of non-association of other operations with cesarean delivery needs to be changed.
CONFLICTS OF INTEREST
The author has no conflicts of interest.